Scroll to:
EPOCHA-AH 1998–2017. Dynamics of prevalence, awareness of arterial hypertension, treatment coverage, and effective control of blood pressure in the European part of the Russian Federation
https://doi.org/10.18087/cardio.2445
Abstract
Aim. To perform a repeated epidemiological study of a representative sample in the European part of the Russian Federation in 2017 and to compare the dynamics of arterial hypertension (AH) prevalence with the effectiveness of blood pressure (BP) control in the population compared to 1998, 2002, and 2007.
Materials and methods. A representative sample of the European part of the Russian Federation was created in 2002 and re-examined in 2007 and 2017. In 1998, a pilot project was performed for examining a representative sample for the Nizhniy Novgorod region.
Results. During 19 years of follow-up, the AH prevalence increased from 35.5 to 43.3%. Te awareness and treatment coverage reached 76.9 and 79.3%, respectively, in 2017. Achievement of the target BP with a single measurement also increased among patients receiving antihypertensive medication from 14.3 to 34.9%. For the treatment of AH, medium-acting antihypertensive drugs are used, ofen at suboptimal doses.
Conclusion. Epidemiological indices of awareness, treatment coverage, and number of effectively managed patients with AH have improved. However, the AH prevalence has increased by 7.8% for 19 years, which indicates inefciency of the primary prevention of this disease.
For citations:
Badin Yu.V., Fomin I.V., Belenkov Yu.N., Mareev V.Yu., Ageev F.T., Polyakov D.S., Artemjeva E.G., Galyavich A.S., Ionova T.S., Kamalov G.M., Kechedzhieva S.G., Koziolova N.A., Malenkova V.Yu., Malchikova S.V., Smirnova E.A., Tarlovskaya E.I., Shechrbinina E.V., Valikulova F.Yu., Vaysberg A.R., Yakushin S.S. EPOCHA-AH 1998–2017. Dynamics of prevalence, awareness of arterial hypertension, treatment coverage, and effective control of blood pressure in the European part of the Russian Federation. Kardiologiia. 2019;59(1S):34-42. (In Russ.) https://doi.org/10.18087/cardio.2445
Hypertension is one of the main risk factors for cardiovascular diseases (CVD), which remains the primary trigger of cardiovascular mortality. The prevalence of hypertension, treatment coverage and effectiveness of blood pressure (BP) control must be determined in the Russian population to understand the problem and identify tactics of reducing cardiovascular morbidity and mortality at the population level. This is dictated by the increasing prevalence of hypertension in many countries and the need for the most complete treatment coverage of hypertensive patients, increasing proportion of patients with effective long-term BP control, that will make the difference in reducing the CVDs and mortality rates.
The prevalence of hypertension in the Europe and the United States is increasing every year [1-3]. The rates of prevalence of hypertension and its increase are significantly different in Europe and the United States, indicating the heterogeneity in economic development of the countries, health systems and hypertension screening programs [3-10].
In the United States, increase in the prevalence of hypertension is associated with a high population-based risk for CVDs [11-13]. In the period from 2009 to 2012, cardiovascular risk >20% was determined in 41.7% of the respondents among the hypertensive patients, 10–20% — in 40,9%, and <10% — in 18.4% [14].
The largest US epidemiological study (NHANES) showed that about 50% of deaths from coronary artery disease (CAD) and stroke are associated with hypertension [15]. In Russia, hypertension is the most common cause of CAD, stroke, congestive heart failure (CHF) [16-18].
Active administration of antihypertensive drugs in patients with hypertension and achievement of target BP levels will make it possible to significantly reduce the cardiovascular risks and mortality [19, 20].
With the high prevalence of hypertension in the Russian population and poor treatment effectiveness, hypertension remains an uncontrolled factor, which determines population-based risks not only for organ damage, but also activates the development of associated clinical conditions [21]. This has determined performing the following epidemiological snapshot of a representative sample of the European Russia.
Objective
Conduct a repeat epidemiological study in the representative sample of the European Russia in 2017 and compare the dynamics of hypertension prevalence and effectiveness of BP control in this population with the 1998, 2002 and 2007 levels.
Materials and methods
In 1998, a pilot study was conducted in the Nizhny Novgorod region, and a representative sample was determined in order to study the prevalence of hypertension and other CVDs. In 2002, a sample consisting of 8 regions (the Kirov, Nizhny Novgorod, Ryazan, and Saratov Regions, the Republics of Chuvashia, Tatarstan, Stavropol and Perm Krais) was created in order to extrapolate the results of the primary outcomes of hypertension treatment effectiveness, obtained in the Nizhny Novgorod region to the European Russia. The representative sample has included 19,503 respondents (≥10 years old). Sampling design and randomization methods used are provided in the “Serdechnaya nedostatochnost" journal [22]. In 2002, the study involved 359 outpatient physicians. 339 therapeutic areas were assessed (94.2% of suggested number) with a total of 8,534 families. The representative sample included respondents registered and residing at randomized addresses. Urban/rural population ratio was 2:1.5. This sample was re-examined in 2007 and 2017.
A questionnaire of 136 questions filled in by a trained clinical physician was drawn up to analyze the prevalence of hypertension, awareness of this disease, the treatment coverage of hypertensive patients, and treatment effectiveness.
The prevalence of hypertension was evaluated by the following criteria: BP randomly measured twice was higher than 140 and/or 90 mmHg regardless of the antihypertensive treatment. Also, the group of hypertensive patients included respondents who had BP below 140/90 mmHg with antihypertensive treatment. This patient group was considered to be effectively treated. Patients were divided into three subgroups: continuous therapy, courses or occasional treatment of high blood pressure.
The study examined CVD therapy received by patients with hypertension. Investigators were not allowed to influence the respondents’ answers and indicated in the questionnaire forms the drugs, which according to respondents were taken for the treatment of CVDs. Drug trade names, doses and frequency of administration were recorded.
Data were processed using a software statistical package. Significance of differences in the non-parametric variables was determined by chi-square test. W-test was used to check the normality of distribution. The drug doses are distributed non-normally, which is why the descriptive statistics used mean, median and quartile range values. The significance of differences between the drug doses were checked by Mann-Whitney test. Differences were considered statistically significant with p<0.05.
Results
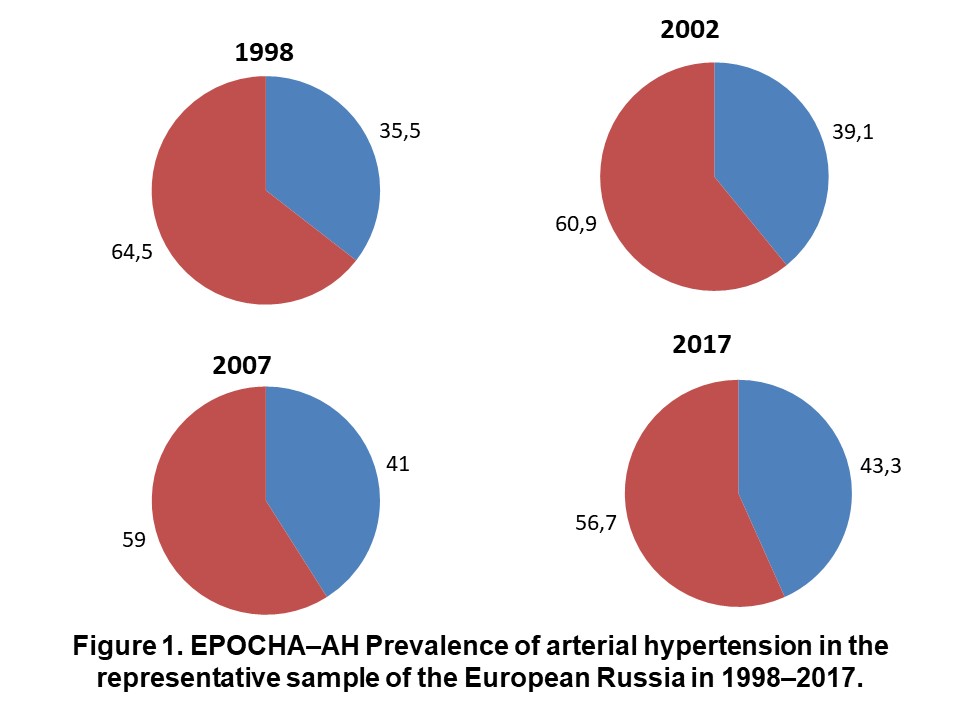
From 1998 to 2017, the prevalence of hypertension in the European Russia increased from 35.5% to 43.3% (p<0,01) (Fig. 1). The number of patients who were not taking antihypertensive drugs among all hypertensive patients decreased significantly from 59.6% to 17.5% (p<0.01). The greatest increase in antihypertensive treatment coverage of hypertensive patients was observed from 2002 to 2007: an average increase in the number of patients taking antihypertensive drugs was 3.5% per year. From 2007 to 2017, the dynamics was significantly slower — 0.95% per year.
Within 19 years of observations, treatment coverage increased 1.96-fold: from 40,4% to 79,3%, (p<0.01). At the same time, the population included more patients with hypertension who, by random measurement of BP, were included in the group of effectively treated patients. In 1998, the group of effectively treated patients constituted 4.7%, in 4 years — 7.5%, in 2007 — 17.0%, and in 2017 the number increased to 30.8%.
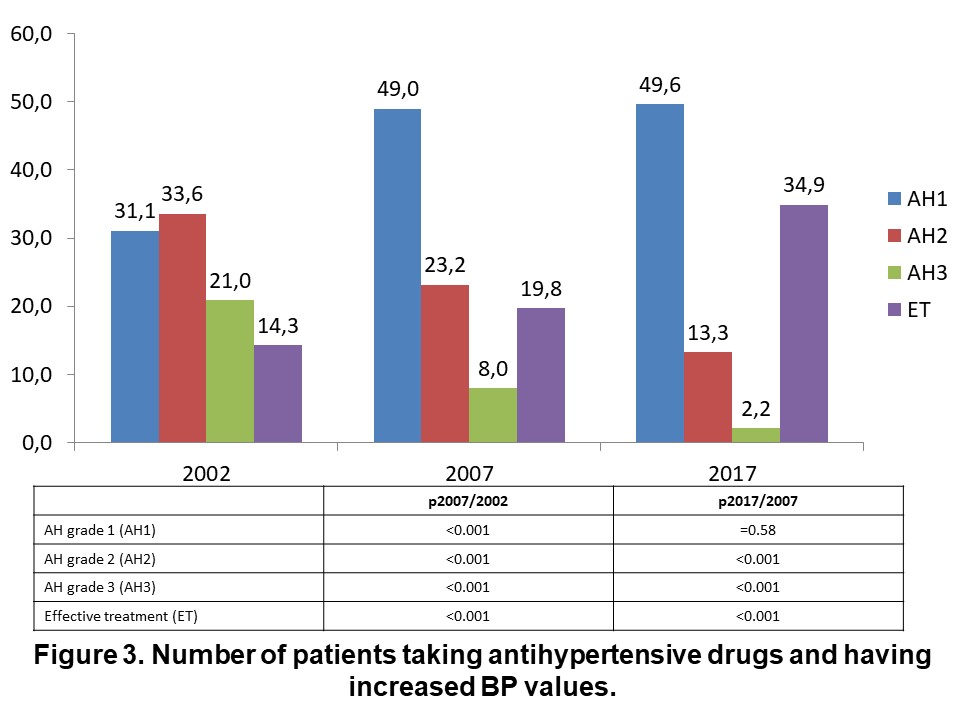
The group of hypertensive patients receiving antihypertensive therapy included slightly more effectively treated patients. In 1998, the proportion of patients with BP below 140/90 mmHg in the population of hypertensive patients receiving medication was 11.5%. In two years, the proportion of such patients insignificantly increased to 14.3% (p=0,086), and in the past 10 years — from 19.8 (p2007/2002<0.01) to 34.9% (p2017/2007<0.01).
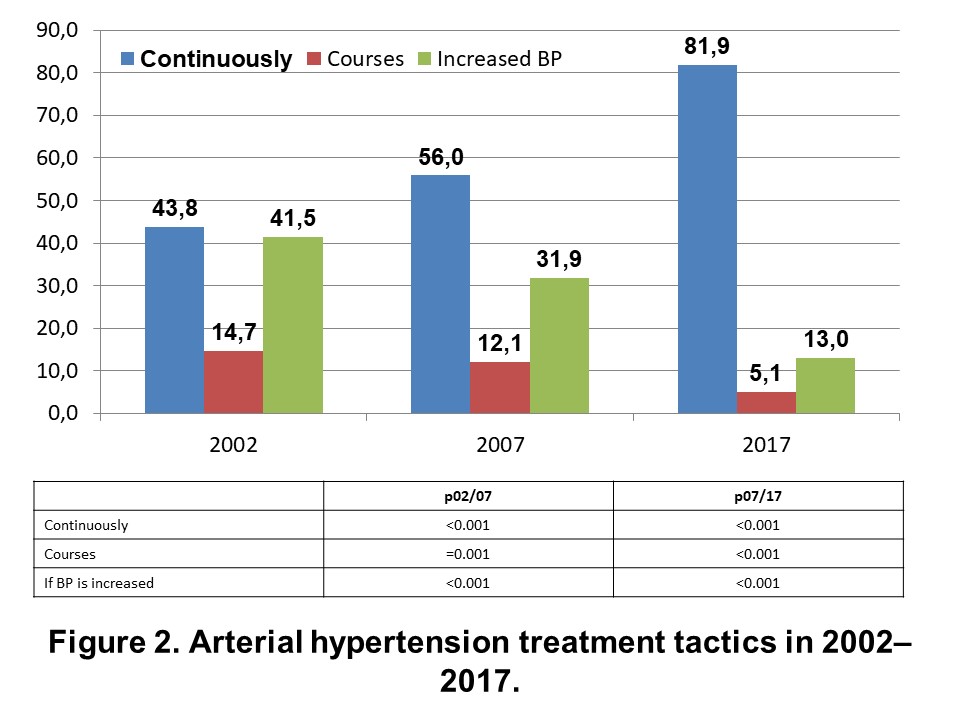
Tactical approaches to the treatment of hypertension during the observation period changed considerably (Fig. 2). The proportion of patients continuously taking antihypertensive drugs increased from 43.8% to 81.9%. At the same time, the proportion of patients taking antihypertensive drugs by courses decreased from 14.7% to 5.1%. A large number of patients remained who take antihypertensive drugs only in case of high blood pressure. In 2002, 41.5% of patients used antihypertensive drugs only with high blood pressure, in 2007 this number decreased to 31.9%. In 2017, the proportion of such patients decreased 2,5-fold to 13.0%.
Tables 2 and 3 provide the most commonly used antihypertensive drugs; the top 10 drugs with the highest frequency of use are included. The treatment failure patients showed a tendency to the preferred use of acetylsalicylic acid drugs, which for the past 19 years have been among the most commonly used medicines. In 2017, the antihypertensive drugs used by patients were mainly diuretics, angiotensin-converting enzyme (ACE) inhibitors and beta-blockers. Interestingly, in the past 10 years, the daily dose of Concor decreased significantly from 7.2 mg to 4.5 mg (p<0.01). Indapamide and enalapril doses did not change significantly in the last 10 years. In 2017, the top 10 most commonly used antihypertensive drugs included long-acting calcium channel blockers (Amlodipine 7.3 mg/day) and sartans (Lozap 72.9 mg/day), however, the recommended average doses were not achieved.
Table 2. Top ten drugs most frequently administered in ineffectively treated AH patients from 1998 to 2017
| Mean | Median | Lower quartile | Upper quartile |
2002 | ||||
Adelphane | 1.5 | 1 | 1 | 2 |
Enam | 10.7 | 10 | 5 | 10 |
Enap | 12.8 | 10 | 10 | 20 |
Atenolol | 65.0 | 50 | 50 | 100 |
Nitrosorbide | 28.5 | 30 | 20 | 30 |
Capoten | 48.3 | 50 | 25 | 50 |
Furosemide | 48.1 | 40 | 40 | 80 |
Aspirin | 147.6 | 125 | 125 | 125 |
Clonidine | 206.3 | 150 | 150 | 300 |
Corvalol | Not applicable | Not applicable | Not applicable | Not applicable |
2007 | ||||
Enap | 14.3 | 10 | 10 | 20 |
Enalapril | 15.9 | 10 | 10 | 20 |
Aspirin | 119.7 | 125 | 75 | 125 |
Indap | 2.5 | 2.5 | 2.5 | 2.5 |
Egilok | 74.5 | 100 | 50 | 100 |
Indapamide | 2.4 | 2.5 | 2.5 | 2.5 |
Concor | 7.2 | 5 | 5 | 10 |
Capoten | 51.6 | 50 | 25 | 75 |
Diroton | 14.7 | 10 | 10 | 20 |
Thrombo ASS | 80.3 | 100 | 50 | 100 |
2017 | ||||
Thrombo ASS | 76.1 | 100 | 50 | 100 |
Cardiomagnyl | 72.9 | 75 | 75 | 75 |
Indapamide | 2.2 | 2.5 | 2.5 | 2.5 |
Enalapril | 14.9 | 10 | 10 | 20 |
Amlodipine | 7.6 | 10 | 5 | 10 |
Enap | 14.0 | 10 | 10 | 20 |
Concor | 4.5 | 5 | 2.5 | 5 |
Bisoprolol | 5.7 | 5 | 5 | 10 |
Lozap | 72.9 | 100 | 50 | 100 |
Atoris | 14.8 | 10 | 10 | 20 |
The structure of the most commonly used medicines in the population of effectively treated hypertensive patients is similar to the structure of the drugs used in the sample of BP control failure patients (Table 3). The most commonly used medicines are acetylsalicylic acid drugs, a conventional dose is 75.1 mg/day. The main antihypertensive drugs are administered in the effectively treated patients in the same or smaller doses than in the treatment failure patients with hypertension. This suggests that more patients in the BP control subgroup had a slight increase in BP, which allowed achieving the target BP levels.
Table 3. Top ten drugs most frequently administered in effectively treated AH patients from 2002 to 2017
| Mean | Median | Lower quartile | Upper quartile |
2002 | ||||
Enam | 8.3 | 5 | 5 | 10 |
Adelphane | 1.3 | 1 | 1 | 2 |
Atenolol | 55.7 | 50 | 50 | 50 |
Nitrosorbide | 30.7 | 30 | 20 | 30 |
Anaprilin | 39.5 | 40 | 20 | 50 |
Enap | 10.9 | 10 | 5 | 10 |
Papasol | 1.6 | 1 | 1 | 2 |
Raunatine | 1.8 | 1 | 1 | 2 |
Aspirin | 147.0 | 125 | 125 | 125 |
Corvalol | Not applicable | Not applicable | Not applicable | Not applicable |
2007 | ||||
Enalapril | 13.3 | 10 | 10 | 20 |
Capoten | 26.5 | 25 | 25 | 25 |
Enap | 10.5 | 10 | 5 | 10 |
Concor | 5.6 | 5 | 2.5 | 5 |
Aspirin | 154.1 | 125 | 125 | 125 |
Indap | 2.4 | 2.5 | 2.5 | 2.5 |
Egilok | 53.4 | 50 | 25 | 50 |
Thrombo ASS | 84.5 | 100 | 50 | 100 |
Indapamide | 2.3 | 2.5 | 2.5 | 2.5 |
Metoprolol | 62.5 | 50 | 50 | 100 |
2017 | ||||
Cardiomagnyl | 73.4 | 75 | 75 | 75 |
Bisoprolol | 6.3 | 5 | 5 | 10 |
Enalapril | 13.8 | 10 | 10 | 20 |
Indapamide | 2.2 | 2.5 | 2.5 | 2.5 |
Concor | 4.4 | 5 | 2.5 | 5 |
Thrombo ASS | 85.6 | 100 | 100 | 100 |
Amlodipine | 7.7 | 5 | 5 | 10 |
Atoris | 16.7 | 20 | 10 | 20 |
Enap | 12.4 | 10 | 10 | 10 |
Lozap | 71.7 | 50 | 50 | 100 |
The number of hypertensive patients who take antihypertensive drugs and don’t achieve the target BP levels was determined (Fig. 3). In the past 19 years, the number of patients with grade III hypertension decreased 21.0% to 2.2%; grade II hypertension — from 33.6% to 13.3%. The proportion of patients who achieve grade I hypertension with the antihypertensive treatment remains large, and this number tends to increase from 31.1% to 49.0–49.6% of the subjects. The figure shows that the Russian patients do not achieve the target BP levels, and half of the patients taking antihypertensive drugs remain within grade I hypertension.
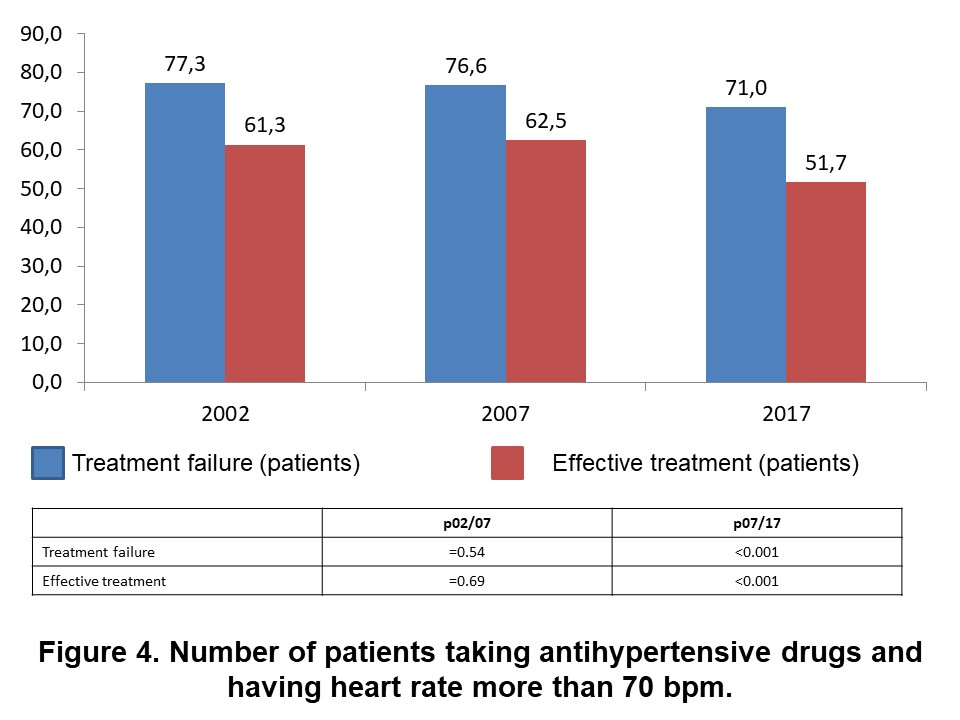
At the same time, we analyzed the heart rate (HR) control in hypertensive patients (Fig. 4). In the subgroup of effectively treated patients with hypertension, the proportion of patients with heart rate above 70 bpm in the whole observation period decreased significantly from 61.3% in 2002 to 51.7% in 2017. The similar pattern was observed in the treatment failure subgroup: the proportion of patients with heart rate above 70 bpm decreased from 77.3% to 71.0%. The number of patients HR control failure increases every year in both groups, which indicates administering inadequate doses of beta-blockers.
Thus, the number of patients who control the BP levels increases, but the list of the most commonly used antihypertensive drugs contains no other long-acting drugs than amlodipine and bisoprolol. This suggests the lack of 24h control of BP levels by most of hypertensive patients. In the past 19 years, the number of hypertensive patients increased by 27.7%, meaning that population-based preventive activities against the development of hypertension are not effective.
Discussion
The prevalence of hypertension in different parts of the world is very heterogeneous, which is why understanding its dynamics and control requires carrying out several epidemiological snapshots and examinations of the treatment coverage in the population of hypertensive patients with definition of awareness and effectiveness of BP control. The most significant results were obtained in the NHANES epidemiological study from 1960 to 2012, which included 6 stages (Table 1). At the first stage (NHES I), the prevalence of hypertension in 1960 was 29.7% with the diagnostic level of BP above 160/95 mmHg [1, 2]. In the following years (NHANES I-III), diagnostic level of BP was above 140/90 mmHg and the prevalence of hypertension in the US population ranged from 20.4 to 32.2% [2]. In 2017, the prevalence of hypertension in the United States reached 46%, as the diagnostic level of BP in the most recent guidelines for the treatment of hypertension [23] was specified as 130/80 mmHg. in 2012, the prevalence of severe hypertension in the US population was 12.3% with BP levels above 160/100 mmHg [24]. In Russia, the prevalence of hypertension has increased significantly from 33.9% (1998) to 43.3% (2017) with diagnostic levels of BP above 140/90 mmHg. Within 19 years, the prevalence of hypertension in all snapshots in Russia was higher than in the United States.
Table 1. Dynamics of prevalence, awareness of AH, treatment scope and effective control of BP according to the studies carried out in the United States and the European Russia
(%) | NHES I (1960-1962) | NHANES I (1971-1974) | NHANES II (1976-1980) | NHANES III Phase 1 (1988-1991) | NHANES III Phase 1I (1999-2000) | NHANES III Phase III (2009-2012) | EPOCHA–AH (1998) | EPOCHA–AH (2002) | EPOCHA–AH (2007) | EPOCHA–AH (2017) |
Prevalence of AH, % | 29.7 | 36.3 | 31.8 | 20.4 | 28.7 | 32.2 | 35.5 | 39,1(р02/98<0,01) | 41.0 (p07/02<0.01) | 43.3 (p17/07<0.01) |
Awareness of AH,% | 53* | 54* | 51 | 73 | 68.9 | 84.2 | 47.7 | 47.6 (р02/98-0.96) | 64.0 (p07/02<0.01) | 76.9 (p17/07<0.01) |
Treatment scope in the AH patient population | 35* | 37* | 31 | 55 | 58.3 | 75.3 | 40.4 | 52.1 (р02/98<0.01) | 69.8 (p07/02<0.01) | 79.3 (p17/07<0.01) |
BP control in the AH patient population, % | 16 | 16 | 10 | 29 | 31.0 | 52.9 | 4.7 | 7.5 (р02/98<0.01) | 17.0 (p07/02<0.01) | 30.8 (p17/07<0.01) |
BP control in the treated AH patients, % | 45 | 42 | 32 | 55 | 53.1 | 69.1 | 11.5 | 14.3 (р02/98-0.09) | 19.8 (p07/02<0.01) | 34.9 (p17/07<0.01) |
In the 1990s, the awareness of hypertension in the US population was 69.2%, the treatment coverage and BP control effectiveness were poor: 52.4 and 24.6%, respectively. By the end of the 20th century, awareness of hypertension in the United States did not change (68.9%), neither did the treatment coverage (58.4%) and BP control (31.0%) [2, 23]. From 2009 to 2012, awareness of hypertension in the United States increased to 84.2%. Treatment coverage of the population in the same period was within 75% (92.4% in the aware population). Single checkup of blood pressure detected the level of BP<140/90 mmHg in 69.1% of patients. This allowed registering the 50% exceeding of effectiveness threshold of the BP control in all hypertensive patients in the United States [24-27]. For 19 years, awareness of hypertension and treatment coverage in Russia has been similar to the US samples, but the population-based BP control effectiveness is almost 2-time lower and is 35% in the treated patients.
The epidemiological studies showed that the BP levels within 120/80–139/89 mmHg significantly increases the risks of CVDs and mortality rates as compared with the optimal BP levels [28]. The most sensitive endpoint in this case is a stroke [29-31]. Reducing BP with antihypertensive drugs to 120-129/80-84 mmHg vs 130-139/85-89 mmHg irrespective of the degree of BP increase >140/90 mmHg before the treatment results in significant decrease in CVDs and mortality rates, OR 1.1-1.5. The blood pressure decrease below 120/80 mmHg increases the effectiveness of antihypertensive treatment [32-35] in reducing the risks of cardiovascular mortality and heart failure. And the control of systolic BP has more prognostic value than the diastolic blood pressure [36].
Our findings showed that with antihypertensive therapy half of the hypertensive patients in the RF remain within I grade BP increase levels (49.6%), less patients have II and III grade BP increase levels (15.5%). For 19 years of observation, the proportion of effectively treated patients with hypertension has increased from 11.5% to 35.0%, but it is worth noting that the treatment is still based on the use of medium-lasting antihypertensive drugs. In the Russian population of hypertensive patients, the proportion of effectively treated patients with hypertension was 27.7%, among which 7.9% of patients taking at least one long-lasting drug.
NHANES III findings show that a significant progress in increasing awareness of hypertension, hypertension treatment and control was observed inbetween the 1990s and the first decade of the 21st century. The experts see the slowdown of growth in the prevalence of hypertension in the United States in the past decade as a result of active primary prevention of hypertension. It was observed that increase in hypertension in respondents aged 20 to 50 years was much less pronounced than 20 years ago. There was a tendency to increase in the number of respondents using a low-sodium diet and controlling body weight. In the NHANES III study, the average systolic and diastolic BP levels were lower in patients with low body mass index. The past 10 years have seen a trend to decrease in the number of patients with a very high body mass index [37].
The Russian study ESSE-RF carried out in 2012-2013 showed a high prevalence (34%) of not only hypertension, but also such risk factors as obesity, dyslipidemia, low physical activity and other. The poor antihypertensive treatment coverage in hypertensive patients was also revealed — 50% [38, 39]. The PYTHAGORAS study showed a high antihypertensive treatment coverage in hypertensive patients (93.6%), but only 62.1% of patients received continuous therapy. The high treatment coverage is explained by the fact that the study included hypertensive patients who sought medical help for high blood pressure [40].
In the Russian Federation, the number of hypertensive patients continues to grow, which suggests low activity in controlling the risk factors. The active prevention in the population may suspend increase in the prevalence of hypertension. Given the small proportion of hypertensive patients with the achievement of BP levels less than 140/90 mmHg, the control of CVDs and mortality rate requires not only the increase in antihypertensive treatment coverage of patients with hypertension, but also improving the BP control with the achievement of target levels in as many patients as possible.
Further national studies on the effectiveness of hypertension treatment are needed to assess the use of modern medicines in the clinical practice. If the current situation of increase in the prevalence of hypertension, poor effectiveness of BP control continues, CVDs morbidity and mortality will remain high. The principles of primary prevention must be implemented to prevent the development of hypertension at the population level and achieve the target BP levels, which is essential to reduce the risk of cardiovascular complications.
Conclusion
1. In the past 19 years, the prevalence of hypertension in the Russian Federation have increased from 33.9% to 43.3%.
2. Awareness of hypertension and treatment coverage significantly improved at the population level, however, BP control in the population of hypertensive patients remains ineffective — 27.7%.
3. One of the main reasons for BP and HR control failure is the use of medium-lasting antihypertensive drugs and insufficient doses.
4. Clinical physicians do not achieve target doses of antihypertensive drugs, which results in the fact that about three quarters of hypertensive patients in this population fail to effectively control the BP levels.
References
1. Burt VL, Cutler JA, Higgins M, Horan MJ, Labarthe D, Whelton P et al. Trends in the prevalence, awareness, treatment, and control of hypertension in the adult US population. Data from the health examination surveys, 1960 to 1991. Hypertension (Dallas, Tex.: 1979). 1995;26(1):60–9. PMID: 7607734
2. Hajjar I. Trends in Prevalence, Awareness, Treatment, and Control of Hypertension in the United States, 1988-2000. JAMA. 2003;290(2):199. DOI: 10.1001/jama.290.2.199
3. Pereira M, Lunet N, Azevedo A, Barros H. Differences in prevalence, awareness, treatment and control of hypertension between developing and developed countries. Journal of Hypertension. 2009;27(5):963– 75. PMID: 19402221
4. Zhou B, Bentham J, Di Cesare M, Bixby H, Danaei G, Cowan MJ et al. Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19•1 million participants. Te Lancet. 2017;389(10064):37–55. DOI: 10.1016/S0140-6736(16)31919-5
5. Macedo ME, Lima MJ, Silva AO, Alcantara P, Ramalhinho V, Carmona J. Prevalence, awareness, treatment and control of hypertension in Portugal: the PAP study. Journal of Hypertension. 2005;23(9):1661–6. PMID: 16093910
6. Chow CK. Prevalence, Awareness, Treatment, and Control of Hypertension in Rural and Urban Communities in High-, Middle-, and Low-Income Countries. JAMA. 2013;310(9):959. DOI: 10.1001/jama.2013.184182
7. Falascheti E, Chaudhury M, Mindell J, Poulter N. Continued Improvement in Hypertension Management in England: Results from the Health Survey for England 2006. Hypertension. 2009;53(3):480– 6. DOI: 10.1161/HYPERTENSIONAHA.108.125617
8. Meisinger C, Heier M, Völzke H, Löwel H, Mitusch R, Hense H-W et al. Regional disparities of hypertension prevalence and management within Germany: Journal of Hypertension. 2006;24(2):293–9. DOI: 10.1097/01.hjh.0000200508.10324.8e
9. Zdrojewski T, Szpakowski P, Bandosz P, Pająk A, Więcek A, KrupaWojciechowska B et al. Arterial hypertension in Poland in 2002. Journal of Human Hypertension. 2004;18(8):557–62. DOI: 10.1038/sj.jhh.1001739
10. Kastarinen M, Antikainen R, Peltonen M, Laatikainen T, Barengo NC, Jula A et al. Prevalence, awareness and treatment of hypertension in Finland during 1982–2007: Journal of Hypertension. 2009;27(8):1552–9. DOI: 10.1097/HJH.0b013e32832c41cd
11. Cheng S, Clagget B, Correia AW, Shah AM, Gupta DK, Skali H et al. Temporal Trends in the Population Atributable Risk for Cardiovascular Disease: Te Atherosclerosis Risk in Communities Study. Circulation. 2014;130(10):820–8. DOI: 10.1161/CIRCULATIONAHA.113.008506
12. Willey JZ, Moon YP, Kahn E, Rodriguez CJ, Rundek T, Cheung K et al. Population Atributable Risks of Hypertension and Diabetes for Cardiovascular Disease and Stroke in the Northern Manhatan Study. Journal of the American Heart Association. 2014;3(5). DOI: 10.1161/JAHA.114.001106
13. Muntner P, Anderson A, Charleston J, Chen Z, Ford V, Makos G et al. Hypertension Awareness, Treatment, and Control in Adults With CKD: Results from the Chronic Renal Insufciency Cohort (CRIC) Study. American Journal of Kidney Diseases. 2010;55(3):441–51. DOI: 10.1053/j.ajkd.2009.09.014
14. Egan BM, Li J, Hutchison FN, Ferdinand KC. Hypertension in the United States, 1999 to 2012: Progress Toward Healthy People 2020 Goals. Circulation. 2014;130(19):1692–9. DOI: 10.1161/CIRCULATIONAHA.114.010676
15. Ford ES. Trends in Mortality from All Causes and Cardiovascular Disease Among Hypertensive and Nonhypertensive Adults in the United States. Circulation. 2011;123(16):1737–44. DOI: 10.1161/CIRCULATIONAHA.110.005645
16. Fomin I. V., Polyakov D. S. β-Blockers: the lack of taskimplementation or the unwillingness of doctors in the Russian Federation to optimize the treatment? System hypertension. 2014;11(1):56-63.
17. Fomin I. V., Polyakov D. S., Badin Yu. V. EPOCHA: Arterial hypertension and coronary heart disease as the main causes of CHF. Effective pharmacotherapy. 2011;12:16-20.
18. Belenkov Yu. N., Mareev V. Yu., Ageev F. T., Fomin I. V., Badin Yu. V., Polyakov D. S. Etiological causes of CHF formation in the European part of the Russian Federation (hospital stage). Russian Heart Failure Journal. 2011;12(6):333-8. DOI: 10.18087/rhf.2011.6.1589
19. Effects of Intensive Blood-Pressure Control in Type 2 Diabetes Mellitus. New England Journal of Medicine. 2010;362(17):1575–85. DOI: 10.1056/NEJMoa1001286
20. Williamson JD, Supiano MA, Applegate WB, Berlowitz DR, Campbell RC, Chertow GM et al. Intensive vs Standard Blood Pressure Control and Cardiovascular Disease Outcomes in Adults Aged ≥75 Years: A Randomized Clinical Trial. JAMA. 2016;315(24):2673. DOI: 10.1001/jama.2016.7050
21. Fomin I. V., Polyakov D. S., Badin Yu. V., Belenkov Yu. N., Mareev V. Yu., Ageev F. T. et al. Arterial hypertension in European Russia from 1998 to 2007: What did we achieve at the population level? Russian Heart Journal. 2016;15(5):369-78. DOI: 10.18087/RHJ.2016.5.2240
22. Mareev V. Yu., Belenkov Yu. N., Ageev F. T., Fomin I. V., Chochlov R. A., Galiavich A. S. et al. Te frst results of Russian epidemiological studies with CHF (EPOCHA-CHF). Russian Heart Failure Journal. 2003;4(1):17-8.
23. Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C et al. 2017 ACC/AHA/AAPA/ABC/ACPM/ AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):1269–324. DOI: 10.1161/HYP.0000000000000066
24. Yoon SS, Gu Q, Nwankwo T, Wright JD, Hong Y, Burt V. Trends in Blood Pressure Among Adults with Hypertension: United States, 2003 to 2012. Hypertension. 2015;65(1):54–61. DOI: 10.1161/HYPERTENSIONAHA.114.04012
25. Fletcher RD, Amdur RL, Kolodner R, McManus C, Jones R, Faselis C et al. Blood Pressure Control Among US Veterans: A Large Multiyear Analysis of Blood Pressure Data from the Veterans Administration Health Data Repository. Circulation. 2012;125(20):2462–8. DOI: 10.1161/CIRCULATIONAHA.111.029983
26. Jaffe MG, Young JD. Te Kaiser Permanente Northern California Story: Improving Hypertension Control From 44% to 90% in 13 Years (2000 to 2013). Te Journal of Clinical Hypertension. 2016;18(4):260–1. DOI: 10.1111/jch.12803
27. Jaffe MG, Lee GA, Young JD, Sidney S, Go AS. Improved Blood Pressure Control Associated with a Large-Scale Hypertension Program. JAMA. 2013;310(7):699. DOI: 10.1001/jama.2013.108769
28. Lewington S, Clarke R, Qizilbash N, Peto R, Collins R, Prospective Studies Collaboration. Age-specifc relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet (London, England). 2002;360(9349):1903–13. PMID: 12493255
29. Etehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Te Lancet. 2016;387(10022):957–67. DOI: 10.1016/S01406736(15)01225-8
30. Guo X, Zhang X, Guo L, Li Z, Zheng L, Yu S et al. Association Between Pre-hypertension and Cardiovascular Outcomes: A Systematic Review and Meta-analysis of Prospective Studies. Current Hypertension Reports. 2013;15(6):703–16. DOI: 10.1007/s11906-0130403-y
31. Huang Y, Su L, Cai X, Mai W, Wang S, Hu Y et al. Association of allcause and cardiovascular mortality with prehypertension: A metaanalysis. American Heart Journal. 2014;167(2):160-168.e1. DOI: 10.1016/j.ahj.2013.10.023
32. Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338(may19 1):b1665–b1665. DOI: 10.1136/bmj.b1665
33. Sundström J, Arima H, Jackson R, Turnbull F, Rahimi K, Chalmers J et al. Effects of Blood Pressure Reduction in Mild Hypertension: A Systematic Review and Meta-analysis. Annals of Internal Medicine. 2015;162(3):184. DOI: 10.7326/M14-0773
34. Tomopoulos C, Parati G, Zancheti A. Effects of blood pressure lowering on outcome incidence in hypertension: 2. Effects at different baseline and achieved blood pressure levels – overview and meta-analyses of randomized trials. Journal of Hypertension. 2014;32(12):2296– 304. DOI: 10.1097/HJH.0000000000000379
35. Xie X, Atkins E, Lv J, Bennet A, Neal B, Ninomiya T et al. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: updated systematic review and meta-analysis. Te Lancet. 2016;387(10017):435–43. DOI: 10.1016/S0140-6736(15)00805-3
36. Benetos A, Tomas F, Bean K, Gautier S, Smulyan H, Guize L. Prognostic value of systolic and diastolic blood pressure in treated hypertensive men. Archives of Internal Medicine. 2002;162(5):577–81. PMID: 11871926
37. National Center for Health Statistics (U.S.). Health, United States, 2013: With Special Feature on Prescription Drugs. Hyatsville, MD. 2014 (5/2014). htps://www.cdc.gov/nchs/data/hus/hus13.pdf. :511
38. Balanova Yu. A., Kontsevaya A. V., Shalnova S. A., Deev A. D., Kapustina A. V., Evstifeeva S. E. et al. Life quality of persons with arterial hypertension in Russia is there relation to treatment? (By data from populational study ESSE-RF). Russian Journal of Cardiology. 2016;21(9):7-13. DOI: 10.15829/1560-4071-2016-9-7-13
39. Muromtseva G. A., Kontsevaya A. V., Konstantinov V. V., Artamonova G. V., Gatagonova T. M., Duplyakov D. V. et al. Te prevalence of non-infectious diseases risk factors in russian population in 20122013 years. Te results of ECVD-RF. Cardiovascular Terapy and Prevention. 2014;13(6):4-11.
40. Leonova M. V., Belousov Yu. B. Results of pharmacoepidemiological study of arterial hypertension in Russia (Pythagoras). Problems of standardization in health care. 2005;4:12-20.
About the Authors
Yu. V. BadinRussian Federation
Minin and Pozharsky square 10/1, Nizhny Novgorod 603950
I. V. Fomin
Russian Federation
Minin and Pozharsky square 10/1, Nizhny Novgorod 603950
Yu. N. Belenkov
Russian Federation
Moscow
V. Yu. Mareev
Russian Federation
Lomonosovskii prospect 27–10, Moscow 119192
F. T. Ageev
Russian Federation
3rd Cherepkovskaya 15a, Moscow 121552
D. S. Polyakov
Russian Federation
Minin and Pozharsky square 10/1, Nizhny Novgorod 603950
E. G. Artemjeva
Russian Federation
Krasnaya Ploshchad 3, Cheboksary 428032
A. S. Galyavich
Russian Federation
Butlerova 49, Kazan 420012
T. S. Ionova
Russian Federation
Krymskaya 15, Saratov 410039
G. M. Kamalov
Russian Federation
Butlerova 49, Kazan 420012
S. G. Kechedzhieva
Russian Federation
Mira 310, Stavropol 355017, Stavropol Territory
N. A. Koziolova
Russian Federation
Petropavlovskaya 26, Perm 614000
V. Yu. Malenkova
Russian Federation
Krasnaya Ploshchad 3, Cheboksary 428032
S. V. Malchikova
Russian Federation
K. Marx 112, Kirov 610027
E. A. Smirnova
Russian Federation
Vysokovoltnaya 9, Ryazan 390026
E. I. Tarlovskaya
Russian Federation
Minin and Pozharsky square 10/1, Nizhny Novgorod 603950
E. V. Shechrbinina
Russian Federation
Minin and Pozharsky square 10/1, Nizhny Novgorod 603950
F. Yu. Valikulova
Russian Federation
Minin and Pozharsky square 10/1, Nizhny Novgorod 603950
A. R. Vaysberg
Russian Federation
Minin and Pozharsky square 10/1, Nizhny Novgorod 603950
S. S. Yakushin
Russian Federation
Vysokovoltnaya 9, Ryazan 390026
Review
For citations:
Badin Yu.V., Fomin I.V., Belenkov Yu.N., Mareev V.Yu., Ageev F.T., Polyakov D.S., Artemjeva E.G., Galyavich A.S., Ionova T.S., Kamalov G.M., Kechedzhieva S.G., Koziolova N.A., Malenkova V.Yu., Malchikova S.V., Smirnova E.A., Tarlovskaya E.I., Shechrbinina E.V., Valikulova F.Yu., Vaysberg A.R., Yakushin S.S. EPOCHA-AH 1998–2017. Dynamics of prevalence, awareness of arterial hypertension, treatment coverage, and effective control of blood pressure in the European part of the Russian Federation. Kardiologiia. 2019;59(1S):34-42. (In Russ.) https://doi.org/10.18087/cardio.2445